Note: This blog contains facts and figures as well as anecdotal stories gathered through conversations with local responders.
According to analysis of provisional data released in 2018, 72,000 Americans died of drug overdoses in 2017. That is more American lives claimed than the entire twenty-year Vietnam War.
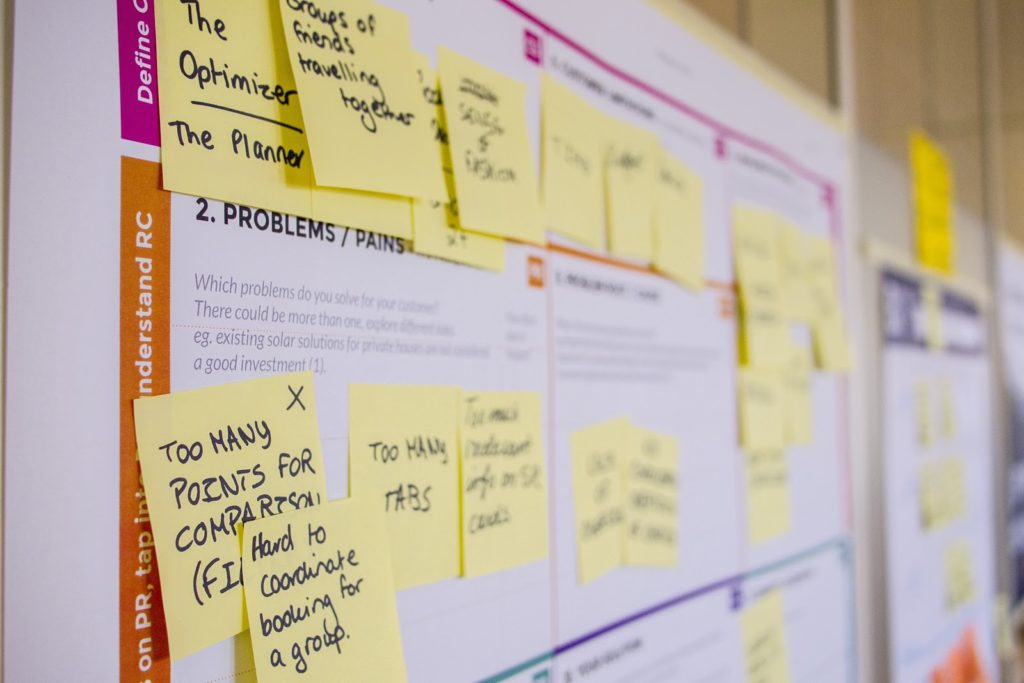
Earlier this year InSTEDD began an effort to support local response to the opioid epidemic, one of the leading causes in the surge of overdose deaths. The start-up work included facilitating an innovation workshop and conducting assessment interviews with public health leaders from hard-hit counties in the USA.
This initial work has focused on experience-sharing and identifying priority challenge areas for innovation. As our team reflects on these conversations, a few key insights have surfaced.
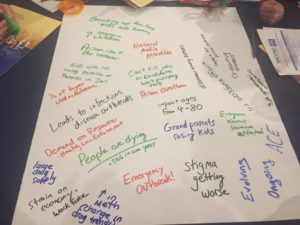
1. The Conversation Starts with Stigma
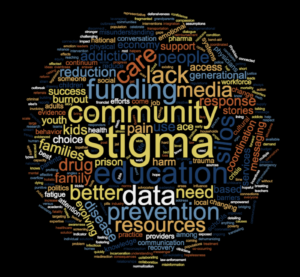
Word cloud of mentioned words by public health officers
Feelings of shame and negative reactions from friends, families and peers are reasons that opioid addictions are kept quiet. The dependence on opioids often begins with a legal prescription, and there may be very little visible appearance of the problem.
Stigma is defined as “a mark of disgrace associated with a particular circumstance, quality, or person.” In the opioid crisis, these marks are words like “junkie,” “druggie” or “addict.” One public health official explained that those who are suffering silently avoid stigma, while those who publicly enter recovery are looked down upon.
Stigma has a significant domino effect. A person who won’t share their problem won’t get help. People avoiding labels and judgment won’t access services or get educated. As an opioid problem becomes known to others jobs are lost, friends are pushed away and families are broken-up.
Almost everyone we speak with knows someone who has been impacted by opioid misuse. Yet these personal stories are often only shared secretly about a sibling, an uncle, parent or close friend.
If we can’t reduce stigma and raise awareness of the epidemic, then we will have no hope of solving this pervasive problem.
2. Beware Unreliable and Misleading Data
Among those we spoke with about the opioid crisis, there was a shared sentiment that the data being reported about the crisis is not entirely accurate. Complex, fragmented, and overburdened state and county health systems make it difficult. Even at the initial intake level, overdose deaths are being miscoded and underreported.
Incomplete data analysis on an evolving crisis can also generate warped conclusions. For example, some counties are proclaiming progress against the epidemic based on data showing a reduction in overdose deaths due to the use of Narcan or Naloxone, an “antidote” drug for reversing overdoses. Getting the drug into the hands of first responders is absolutely critical, but doesn’t necessarily show we are winning the battle against opioid misuse.
A recovery specialist shared with me that out of the 200 overdosing people to whom he had given Narcan in the past month, only one went on to receive recovery services. The result of reversing overdose deaths without recovery creates data that shows a dip in overdose deaths, but also a rise in the total number of overdoses.
The current unavailability of good data on the epidemic points at a crisis that is “at the end of the beginning, not the beginning of the end.” Starting a successful fight against the epidemic will require sound data collection, strong evaluation and open sharing of results.
Strong data and analysis builds empirical evidence on what works, and helps responders avoid the pitfall of ideas that sound good, but lack impact.
3. Accessing Care is a Common Problem for Various Reasons
Across the conversations with responders in different states, a common theme was the difficulty in connecting individuals in need of treatment to support and care.
In some places, especially where services are a significant distance away, simply accessing transportation is the barrier. In other areas, determining which services are available and if an individual fits the criteria for receiving services is an obstacle.
For example, consider the challenge of finding a bed for multi-day medically assisted treatment (MAT) during the initial withdrawal stage of recovery. The demand for these MAT beds is often so high that locating where beds are available, what type of insurance they take, and other criteria for acceptance can take an unreasonable amount of effort. We heard stories of individuals calling dozens of health centers or traveling hours for care, only to arrive and find that previously open beds had been filled, or that they did not meet certain criteria.
In other communities the reality is that linkage to care is difficult because needed services are physically non-existent. In this case, linkage to care might mean access to a hotline, Facebook group or other online peer-support service.
Whether digital or in-person, linking individuals into immediate and long-term recovery support will be a critical innovation area for turning the tide on the deadly opioid epidemic.
In the weeks ahead, InSTEDD will continue its assessment of the opioid crisis, looking for opportunities to bring innovation and open source technologies to aid in the local response. Stay tuned to InSTEDD.org for the latest news and blogs.