Evidence-based, life-saving, and cost-effective treatment exists to combat opioid use disorder, which has reached epidemic levels in the US. The catch? Thousands of people face discouraging roadblocks every day while trying to access this care.
Medication assisted treatment (MAT) is one example of a treatment option that has been proven to help people recover from opioid use disorder (OUD).
If an individual struggling with OUD is ready to quit, overcoming the withdrawal symptoms from these powerful drugs can be extremely painful and even dangerous. To help people focus on recovery, the FDA has approved several medications that ease debilitating withdrawal symptoms and cravings. MAT programs specialize in prescribing these medications in safe doses, ideally alongside medical, behavioral, educational, and other types of treatment.
MAT is an evidence-based intervention making a significant difference for individuals struggling with OUD, and is encouraged by national health organizations, front-line health providers, and the Surgeon General. States are beginning to enhance their MAT program offerings, in spite of pervasive and ill-informed stigmas against using medications to counter medication-addiction.
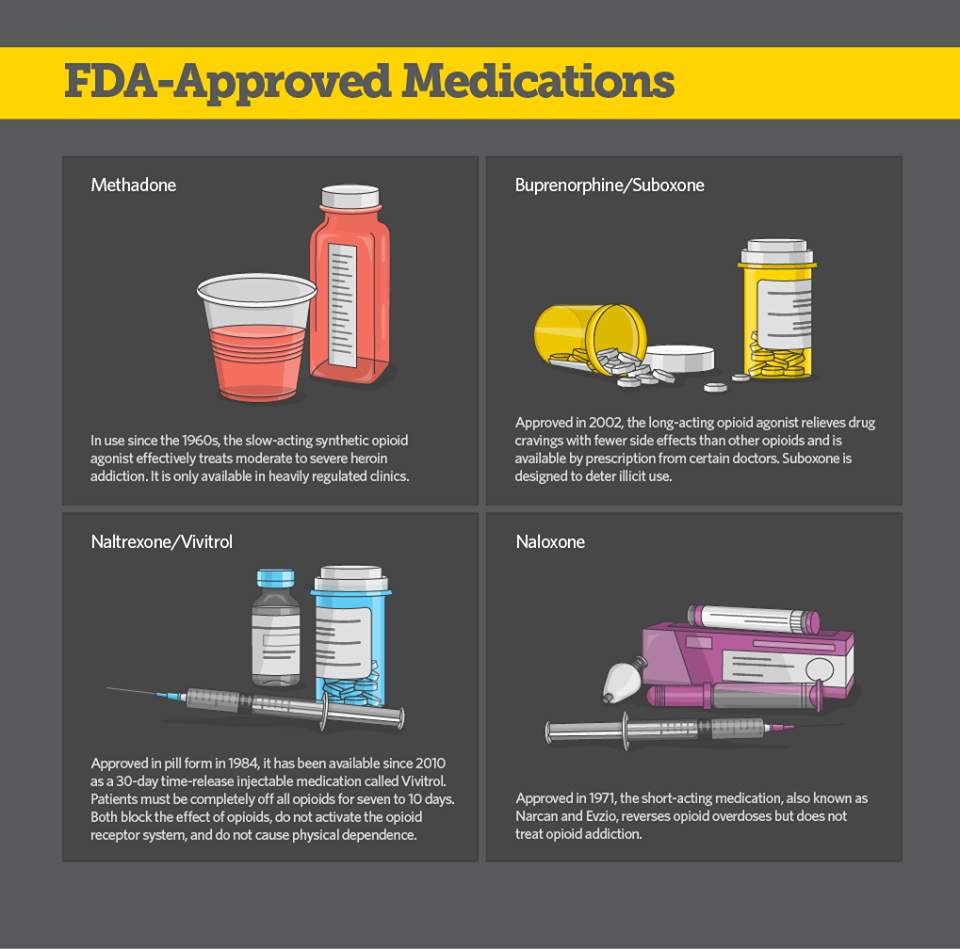
The FDA-approved MAT drugs are methadone, buprenorphine, and naltrexone for treatment, and naloxone for overdose. Image credit: https://www.ktoo.org/
One executive at a MAT treatment provider we’ve spoken with is Anthony Bellot of CleanSlate, who shares that, “MAT is important because it works. The evidence is clear that patients who receive medication as part of their treatment program have an increased chance of staying in recovery. Medication reduces the likelihood of relapse and keeps patients safer when relapses do occur.”
So what is preventing individuals from getting into MAT treatment programs? Here are 3 of the most common barriers we’ve heard from interviews with MAT providers and workshops with county health coalitions and other treatment providers:
Barrier #1: Availability
There are significant gaps in MAT capacity compared to national need. Thirty million Americans live in counties where zero physicians have the required federal waiver to prescribe buprenorphine. Buprenorphine is one of the most accessible MAT options as it can be prescribed and dispensed in physician offices, unlike methadone treatment which must be administered in a highly structured clinic. A national needs assessment in 2012 showed that 96% of states had opioid abuse or dependence rates higher than their buprenorphine treatment capacity rates. This lack of MAT availability not only makes it difficult to begin treatment but also to continue and complete the course of treatment without interruption.
Increased funding for expanding MAT services and providing greater incentives for care providers could help with availability issues. CleanSlate notes that more funding is also needed to provide patients “not only with a prescription for medication, but also with truly individualized treatment plans that include the psychosocial support patients need.”
Other local providers report that many physicians are unaware of the process to get licensed to prescribe MAT, and those that are licensed are often slow to start enrolling patients.
For licensed physicians and facilities, many offer inpatient beds on a first-come, first-served basis and turning people away from treatment is common after they have reached capacity. Outpatient services and referrals to partner programs are some current backup options, but are not universally offered. For people traveling significant distances to access MAT programs, capacity issues are a harrowing deterrent in initiating and continuing care.
Opportunities to increase availability:
- Improve outreach and education to physicians about the MAT waiver and licensing process.
- Create online or phone resources that show real-time availability of inpatient and outpatient services at licensed facilities.
- Increase funding and incentives for care providers to offer MAT.
- Some states, such as Vermont and California, have implemented Hub and Spoke models to enhance their MAT capacities. Share learnings and best practices from such initiatives in national consortiums.
Barrier #2: Access
Finding and accessing these sparse MAT offerings are significant challenges for people seeking care. Misinformation, decentralized resources, transportation barriers, and a lack of general awareness of what MAT entails can keep people from seeking treatment. For example, some people believe seeking assistance with OUD means checking in to an inpatient detox program. While for some people this is the most helpful option, outpatient and other flexible options also exist that allow people to stay in their own homes while still receiving high-quality treatment.
Varying eligibility issues also stand in the way of accessing treatment. For instance, in California, patients who are publicly insured must prove that they have tried detoxing two or more times and subsequently relapsed before the state will pay for treatment with methadone or buprenorphine. Making these issues transparent ahead of time for people seeking treatment in an online or phone resource could make a huge difference in accessibility and morale.
Opportunities to improve access:
- Develop user-friendly resource maps and referral systems for people to locate services.
- Create centralized, evidence-based information hubs with FAQs about MAT and other opioid treatment programs.
- Offer online or phone-based questionnaires for people to determine which facilities would be the best fit for their specific needs and circumstances.
Barrier #3: Stigma
Stigma around seeking treatment for OUD is ingrained in many communities. People report experiencing more judgement when seeking support or treatment than when staying quiet about their addiction. This societal factor can dissuade people from seeking care, as they do not want to be alienated or perceived differently by their communities.
Opportunities to reduce stigma:
- Create safe online spaces for people to seek support and community.
- Educate communities and medical providers about OUD and MAT.
- Revise existing policies that criminalize people seeking treatment for OUD.
If you or someone you know is in need of MAT, here are some resources to help locate services:
- FAQ and resource locator for adults and youth from the National Institute on Drug Abuse
- SAMHSA’s list of physicians certified to prescribe buprenorphine in each state
- SAMHSA behavioral health treatment locator
- SAMHSA’s national help hotline 1-800-662-HELP (1-800-662-4357)
InSTEDD is building a national consortium of care providers, government actors, health coalitions, and other OUD stakeholders to design scalable, adaptable responses to this epidemic. If your organization is interested in joining, please fill out this form.
We’d like to thank CleanSlate for their on-the-record comments about MAT. You can find more information about their organization here.
By Katherine Sziraczky
InSTEDD Global Ambassador USA