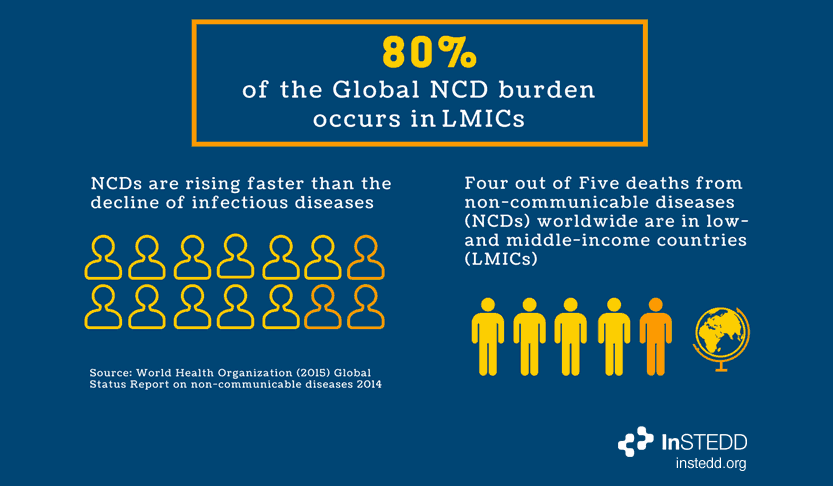
Non Communicable Diseases (“NCDs”) are the world’s leading cause of mortality and morbidity, but popular understanding still links LMICs (low to middle income countries) with infectious diseases. Until the threat of NCDs is better understood, there cannot be a comprehensive response.
17 million NCD deaths occur before the age of 70, and 87% of deaths are estimated to occur in LMICs. Health systems in LMICs have not fully adapted to respond to the NCD disease threat. As a result, there is a high rate of non-compliance with prescriptions for chronic diseases (compliance is 50% in developed countries and much less in LMICs), which is a major cause of treatment failure.
The magnitude of these diseases continues to grow in LMICs as work patterns change (i.e. office work and sedentarism) alongside greater availability of convenient and well-marketed junk food. These factors lead to less healthy lifestyle choices. Existing studies about the impact of these lifestyle changes are patchy and limited in scope, resulting in an increasing need for more detailed research into this health issue.
Until recently, the primary means of collecting data for public health studies has been face-to-face national household surveys conducted at roughly 5-year intervals. This methodology requires extensive time and resources, and suffers from huge gaps between when the data is collected and when it is released (and can therefore be acted upon). In a rapidly changing disease landscape, this approach simply cannot scale at the speed needed to address these issues in time.
Perhaps the most famous example of this approach is the Framingham Heart Study, an ongoing cardiovascular cohort study on residents of the town of Framingham, Massachusetts. Next year, it will celebrate its 70th anniversary, and is now on its third generation of participants. The Framingham study has provided substantial insight into the epidemiology of cardiovascular disease and its risk factors, but relies on data collection methods that require researchers to visit the community in-person. However, researchers are exploring alternatives to this traditional methodology. Common technology, such as mobile phones, have the potential to drastically reduce the time needed to collect data.
The NCD Mobile Phone survey, part of Bloomberg Philanthropies Data for Health Initiative, allows researchers to survey NCDs through different channels, languages and modes; i.e. interactive voice response (IVR), short message service (SMS), mobile web, and more. The survey tool, “Surveda”, is open-source and founded by the consortium running the survey (CDC, CDC Foundation, RTI International and InSTEDD). This first-of-its-kind multi-country, multi-modal mobile phone survey will provide timely data on NCDs and risk factors, which can be used as a guide for public policy.
The consortium will work to support national surveys and analyze the information from Surveda. The consortium behind the NCD Mobile survey project believes that enabling researchers to use a variety of methods to gather data and compare trends in different parts of the world will provide a broader perspective of the true impact of NCDs.
21st century problems require 21st century solutions. A more connected and communicative world should be embraced by researchers, governments, NGOs and other public health policy stakeholders, who are working to tackle deeply rooted problems like NCDs.
Featured image credit: Internews Europe Flickr