By Dr. John B. Niwagaba
Following the paper trail of patient data
At the end of every month at the hospital where I work in Kampala, Uganda, I, like every other doctor at the hospital, am responsible for conducting routine Morbidity and Mortality (MM) audits. This is a review of all patients admitted to the unit in that month, including the reason for their admission, and the percentages of those who lived and those who died. This audit provides vital analysis on disease trends as well as the causes of death to inform policy changes for improved care. While these stats are exciting, the process of compiling this data is daunting.
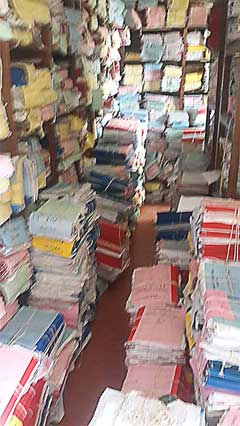
The Hospital Records Room, filled with folders of patient data
The doctors charged with preparation of the month`s audit usually begin their journey in the records store, a vintage building with poor lighting at the far end of the hospital complex adjacent to the mortuary. Files of papers are piled together, in stashes tied with sisal ropes organized in units, which are defined by the date of admission of the patients. Files from all departments – as long as the people were admitted on the same day – are kept together in one mound. The store is arranged supermarket style, and strolling through the walkways with cobwebs and silence is reminiscent of a haunted mansion scene from a horror movie.
The far end of the building looks undisturbed with thick layers of dust, as the files from the 80s and 90s have not been touched in a long while. Painstakingly the doctors review stack after stack for the whole month, filling in Excel sheets and later analysing the data to generate indices like mortality rate, number of deaths in the first 24 hours, and common reasons for hospitalization as well as causes of death.
Sifting through the stacks for patient care
The most important record we have is the Patient Chart, which is a booklet containing the detailed story of a person and their illness. This is the way data is recorded and stored; in these booklets. Doctors record detailed notes and personal details, including the symptoms that brought the patient to the hospital in the first place, past medical history, and also a social history to help make a diagnosis.
This is usually followed by a full body examination, and then a doctor makes a tentative diagnosis and starts emergency treatment while awaiting confirmatory results from imaging or the laboratory. A patient is then followed up on the ward daily, monitoring progress until the patient improves, goes home, gets worse or dies.
For patients who spend a long time in hospital, sometimes up to 3 or 4 booklets will be used. This is a lot of data, most of which is largely inaccessible. This data is property of the hospital and is not freely sharable with the patient or their primary caregivers, save for small summaries on discharge forms that the patient or attendant can leave the hospital with.
Most hospitals in Sub-Saharan Africa still use these paper records of their patients. Even the summaries sent to their Ministries of Health are in a hard paper form. A few hospitals have started digitizing sections of their health data, but the road to paperless medical data system remains riddled with encumbrances.
How can we accelerate and prioritize digitization efforts for improved health in Uganda?
How then can we have a complete loop digitalized system that can collect health data from different levels of health care givers into a common pool, where it can be analysed and interpreted in real time to offer quick decision-making? How can this information be shared with other relevant authorities like police, immigration and other government parastatals to provide round-the-clock surveillance of disease, outbreaks, crime and other health-altering dynamics of our society?
To get rid of the paper-based system, there are multiple challenges at 3 major strategic points that have to be unlocked. They are both ideological and structural and include;
Empower Patients: Patients value and idolize the hard-copied, hand-written treatment forms from their doctors. My own father-in-law complained to me about a ‘young doctor’ who, instead of listening to his complaints, kept typing away at his computer. My attempts to explain to him that he was recording his story fell on deaf ears. He still treasures the experience of his aging doctor who, after a lengthy chat, gives him a hand-written treatment form. He even showed me the stash of these forms as ‘evidence’ of the good old days “when doctors were still doctors”.
In a country where a person can buy almost any drug over the counter, this treatment form offers an added advantage for patients to access them without paying more consultation fees, especially for chronic diseases. Obviously, unlike my father in-law, most patients lose their forms and on subsequent review even the doctor cannot remember what was prescribed before. It’s even worse when most patients hop from doctor to doctor, leaving no trail of their medical history.
Incentivize Hospitals: The setup and patient flow in most hospitals makes it cumbersome to digitalize patient information. While current attempts have been made to electronically register patients, run outpatient department and send orders to the laboratory and imaging units, the inpatient section remains largely out of reach.
Ironically, most of the hospital data is taken from admitted patients as there is more time with each patient through ward rounds and senior consultations. It would require a large labour force to transcribe all of that data into digital content, and that is costly and time-consuming. In addition, doctors themselves abhor the process of recording data electronically. They complain about it being time consuming and impractical in busy public hospitals, and especially so since they get no extra pay for the additional work.
Engage Government: The overseeing Ministry of Health is itself analogue, usually receiving summarized health data on printed forms, which are typically filled in with ink. Most of the HMIS forms for disease surveillance and reporting are hard copies. Relevant laws and policies to streamline digital health are still in short supply and the perennial song of underfunding compounds the problem. Even the little work done by development partners and donor agencies is fragmented and doesn’t offer real tangible value.
Open-Source Collaboration can lead to a resolution
At present day, the change from paper-based reporting to fully digital reporting feels very far off due to the obstacles listed above. However, I’ve also listed ways that thought leaders, contributors, and end-users can collaborate and communicate in order to take what is a fragmented data system and make it whole. There are technological advances that I’ve touched on, and once we can get the necessary stakeholders together, working through obstacles and considering alternatives over the course of several days together, I believe that we can arrive at a resolution in the near, and not too distant, future.